For Healthcare Professionals
5. Hospital Acute Care
The Final Push
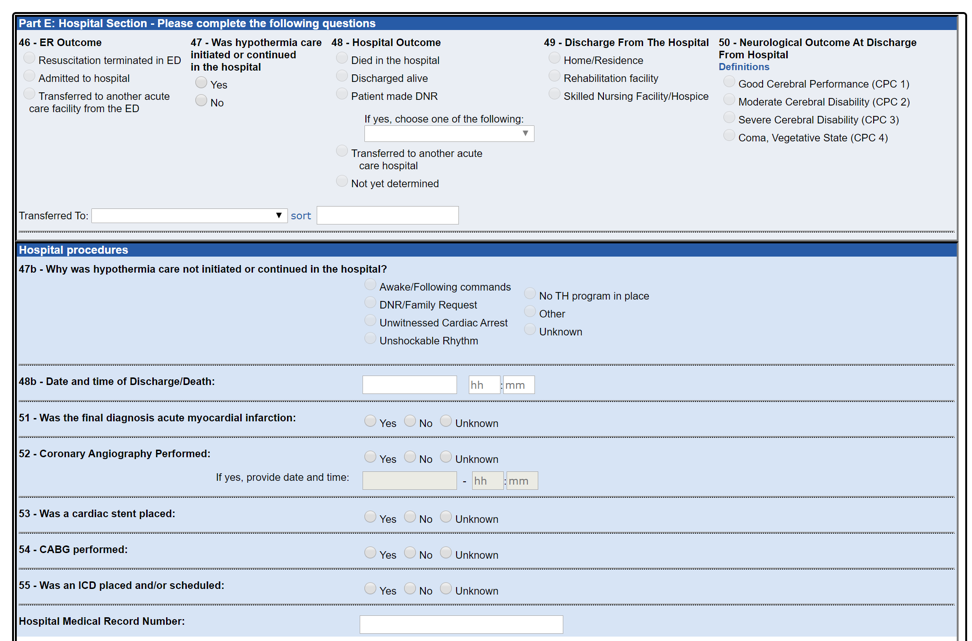
Patient care information indicates whether certain interventions occurred. This includes details related to targeted temperature management hypothermia, coronary angiography, coronary artery bypass graft, cardiac stent, and/or implantable cardioverter defibrillator. Barriers to certain procedures such as hypothermia are tracked, for example, if patients are awake and following commands, a DNR request exists, the cardiac arrest was unwitnessed, the heart rhythm is not responsive to defibrillation, no hypothermia resources are available, or other known or unknown barriers were present.
Outcome information includes both emergency room determination and final hospital discharge status. For emergency room outcome, data relates to whether patients had resuscitation efforts terminated upon arrival, were admitted to the hospital, or were transferred to another acute care facility. Hospital outcome covers patients’ DNR status, and whether they died in the hospital, were discharged alive, or were transferred to another acute care facility. Finally, both known and unknown cases of acute myocardial infarction as final diagnosis are tracked.
For survivors, additional information is captured on whether patients were discharged from the hospital to a residential location, rehabilitation facility, or skilled nursing or hospice care facility. Neurological outcome at discharge time is also indicated based on cerebral performance categories (CPC), with CPC 1 for good cerebral performance, CPC 2 for moderate cerebral disability, CPC 3 for severe cerebral disability, and CPC 4 for comatose or vegetative activity.
As Texas-CARES participants, hospitals are in a unique position to drive quality improvement efforts both in the final ink and throughout the rest of the chain of survival by completing the cardiac arrest picture with final patient outcomes.